In recent years, Singapore has experienced a significant rise in the cost of living, creating a multitude of challenges for its residents. As the city-state continues to develop and expand, the financial burden on individuals and families has intensified, leading to notable mental health repercussions. This blog post explores the intersection of the rising cost of living and mental health problems in Singapore, highlighting the need for a comprehensive approach to address this pressing issue.
Singapore’s Economic Landscape
Singapore is renowned for our rapid economic growth and high standard of living. However, while this success creates prosperity, it also creates other challenges that accompany success. For example, the prices of essential goods and services, including housing, healthcare, and education, have increased, making it increasingly difficult for many Singaporeans to maintain their standard of living. The cost of post-pandemic private housing has surged, with a corresponding increase in rental prices. Additionally, healthcare costs have risen, and education expenses continue to climb, adding to the financial strain on families.
The Psychological Toll
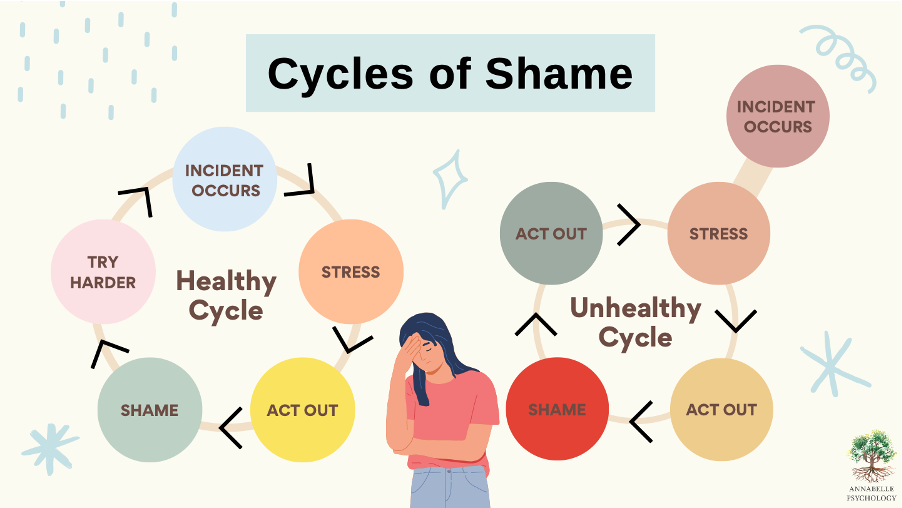
The financial pressures associated with the rising cost of living have led to a significant increase in stress, anxiety, and depression among Singaporeans. The constant worry about meeting daily expenses, paying off rent or mortgages in the most expensive city to live in in the world, or paying for a university education can be overwhelming. These financial concerns can contribute to chronic stress, which, in turn, exacerbates mental health issues.
Stress and Anxiety: The fear of not being able to make ends meet can lead to chronic stress. Many individuals find themselves working longer hours or taking on multiple full-time jobs to cope with financial demands. This relentless pursuit to achieve what is deemed by many to be financial stability in Singapore can result in burnout and severe anxiety.
Depression: Financial instability and the inability to provide for one's family can lead to feelings of hopelessness and depression. The stigma associated with financial struggles may prevent individuals from seeking help, further deepening their mental health issues
Social Isolation both in individual and family settings: The high cost of living can limit social activities and recreational opportunities, leading to social isolation. This might surprise man -: but when people cut back on social interactions to save money, they may lose valuable support systems, which are crucial for mental well-being. This may be especially true in families where both parents juggle working full-time jobs and parenting duties. Unlike in Western societies, parents here in such situations often maintain very few social engagements either to save on discretionary spending or to look after their children.
Vulnerable Populations
Certain groups are more vulnerable to the mental health impacts of the rising cost of living:
Low-Income Individuals or Families: Those with fewer financial resources find it harder to buffer against rising costs. The struggle to afford basic necessities often leads to heightened stress and anxiety.
Elderly Residents: Older adults on fixed incomes may find it challenging to keep up with rising expenses. Social isolation and financial dependency can significantly affect their mental health.
Young Adults: Young professionals and families who are have not achieved financial stability may find it difficult to achieve financial independence within a short span of time. Given the rising costs of raising children in today’s world, the pressure to secure housing and provide for future children can lead to significant stress.
Addressing the Issue
To mitigate the mental health impacts of the rising cost of living, a multi-faceted approach is required:
Government Initiatives:
The Singapore government has introduced several measures to help alleviate financial pressures. For instance, the Enhanced CPF Housing Grant (EHGH) provides up to SGD 80,000 to first-time buyers of new or resale flats. Additionally, the Workfare Income Supplement Scheme (WIS) offers financial assistance to low-wage workers.
Healthcare subsidies, such as the CHAS (Community Health Assist Scheme), help reduce out-of-pocket medical expenses for lower- to middle-income Singaporeans. The CHAS Green scheme was also introduced in Nov 2019 to allow all chronic patients, regardless of income, to enjoy CHAS subsidies for mental illnesses under the Chronic Disease Management Programme (CDMP) (namely major depression, anxiety disorders, bipolar disorder, and schizophrenia) at CHAS GPs clinics. Currently, patients can also withdraw up to $500 per year from their MediSave for the outpatient management of conditions under the CDMP.
Mental Health Support
Increasing access to mental health services is crucial. This means, in part, making mental healthcare affordable. The Ministry of Health has expanded the National Care Hotline to provide psychological support and counselling.
Non-governmental organizations such as Samaritans of Singapore (SOS) provide crisis support and suicide prevention services, ensuring that those in distress have someone to turn to.
Leading a Values-based Life
But I’ve saved the best for last. I want to share a little about what a value-based life is, and what it means for us as unique individuals.
When individuals align our lives with our core values, we often find greater purpose and meaning, which acts as a psychological anchor, helping us navigate financial challenges more effectively. This alignment builds inner strength and resilience, enabling better coping mechanisms against stress and anxiety caused by financial pressures.
For example, emphasising values like community and relationships leads to stronger support networks, providing both emotional and practical support during tough times. These networks reduce feelings of isolation and stress, and promote mutual aid practices where communities share resources, lessening individual financial burdens.
Values-based living also encourages reduced materialism and simplified living. By focusing on contentment and gratitude, individuals find satisfaction with less, lowering the psychological impact of financial constraints. This shift towards mindful spending based on core values helps individuals feel more in control of their finances, reducing stress.
Furthermore, values like self-compassion and acceptance improve emotional well-being. Being kinder to oneself during financial hardships and accepting the situation without undue stress allows individuals to focus on proactive measures rather than ruminating on financial woes.
Lastly, living according to long-term goals aligned with personal values helps maintain focus on broader life objectives, rather than being overwhelmed by immediate financial challenges. This alignment creates a sustainable and fulfilling approach to managing money, reducing financial stress and anxiety over time.
Solving the Impact of Rising Costs on Mental Health
The rising cost of living in Singapore is an undeniable reality that significantly impacts mental health. As financial pressures mount, so do the levels of stress, anxiety, and depression among residents. Addressing this issue requires a collaborative effort from the government, healthcare providers, and the community. By implementing supportive policies and promoting mental health awareness, Singapore can help its residents navigate these challenges and foster a healthier, more resilient society.
More importantly however, the solution does not only lie from external sources, but more importantly, must come from within ourselves. Living a values-based life offers a robust framework for reducing the mental health impacts of rising costs. By focusing on what truly matters, building strong support networks, and cultivating resilience, individuals can navigate financial challenges more effectively and maintain their mental well-being. Emphasising values over materialism and practicing mindful spending and being are practical steps that can make a significant difference in one's financial and emotional health.
Prosperity does not have to come at the expense of health or mental health.
Singapore can work towards a future where all have the opportunity to thrive economically and emotionally.