THERAPIES
Dialectical Behavior Therapy (DBT)
Credit: UC San Francisco (UCSF)
Developed on the back of the scientifically validated Cognitive Behavioural Therapy (CBT) model, Dialectical Behaviour Therapy (DBT) is a cognitive-behavioural therapy developed specifically for addressing complex mental disorders such as Borderline Personality Disorder (BPD).
DBT has also been shown to be highly effective in addressing suicidal behaviour.
Biosocial Theory and the effectiveness of DBT on BPD
The biosocial theory of borderline personality disorder postulates that individuals with BPD have a biological predisposition to emotional vulnerability. Emotional vulnerability can be understood as a measure of an increased sensitivity to emotional stimuli and an atypically heightened experience of emotion. Individuals who experience such vulnerability also face difficulty with emotional regulation.
Others who do not understand the difficulty of such experiences thus tend to invalidate the problems that such individuals face with emotional regulation. The negative environmental feedback can push the vulnerable individual toward developing BPD. This may manifest as increased emotional dysregulation and the use of maladaptive coping mechanisms.
The Three Cornerstones of DBT
DBT adopts three cornerstones in the management of BPD:
DBT Cornerstone 1 - Validation
Validation refers to the clinician's role and responsibility in validating the sufferer’s emotional experiences and reactions. This extends to acknowledging that the problems the client experiences are difficult and that their behaviours, maladaptive or not, are understandable - which often may not be accepted by the client’s family or friends. Through validation, the clinician first aims to recalibrate the negative environmental feedback that the client has been experiencing for most of his or her life.
Credit: Annabelle Psychology
DBT Cornerstone 2 - Dialectics
DBT borrows the philosophical idea of “dialectics” which refers to the understanding that everything consists of opposites. Any position thus has both a thesis and an antithesis. What is essential for balance is therefore a synthesis of the two. DBT exercises this philosophy in recognising the need for synthesis between:
Ψ accepting one’s emotional experiences and reactions and
Ψ changing dysfunctional behaviours and responses.
For example, while a clinician would validate a particular self-harm behaviour that a client engages in (ie. to let them know that it is a reasonable response to emotional distress), they would also have to identify that there exists other less consequential coping methods. Ultimately, DBT repeatedly conveys the idea that there are more adaptive methods to address their problems.
DBT Cornerstone 3 - Mindfulness
Mindful practices encourage the individual to focus on the present, thereby simultaneously decreasing anxiety and increasing self-awareness. This is effective for clients with BPD who have to endure tumultuous emotions and negative environmental feedback. Mindfulness can also be understood as a kind of acceptance-based strategy.
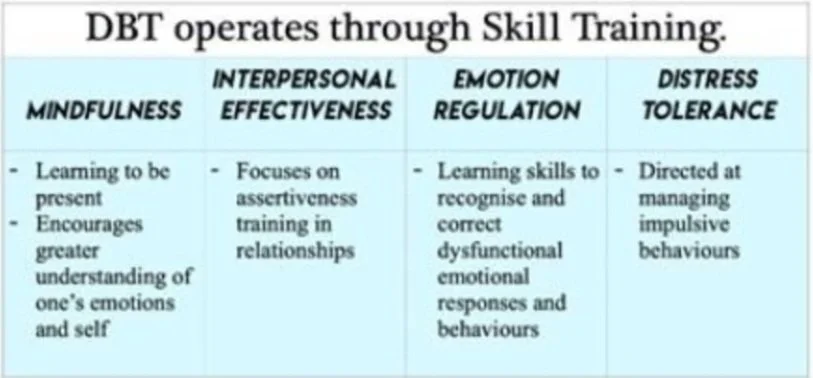
DBT Skills Training
The DBT practitioner then harnesses these cornerstones and works with clients to empower them with the four essential skills that will help them adjust and cope with behavioural issues.